Why Fungal Acne Is No Fun
Ever had acne that seems resistant to any type of treatment, no matter what you tried? Turns out you may have fungal acne. Fungal acne is a bit of a trickster—it looks like your regular run of the mill acne but is resistant to the same benzoyl peroxide or salicylic acid treatments. Knowing the cause of fungal acne helps in knowing how to treat and prevent it.
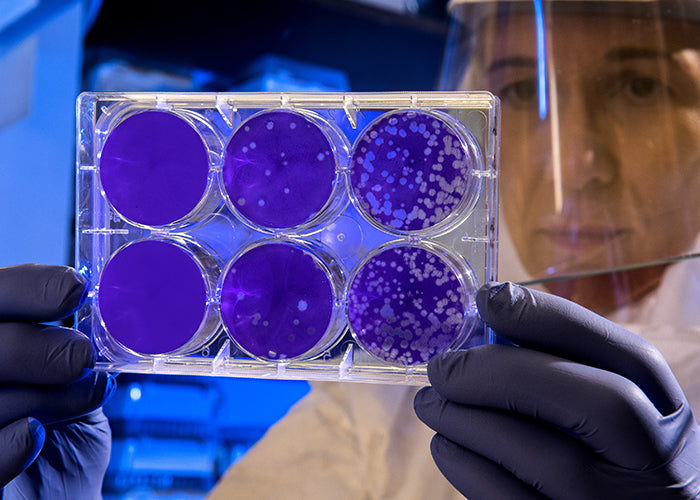
The reason is fungal acne (or as it is technically known pityrosporum folliculitis or malassezia folliculitis) is resistant to regular acne treatments is because n’t caused from hormones or bacteria like most acne. Fungal acne is caused from a yeast that lives on everyone’s skin and when the natural yeast (malassezia) is unbalanced the result is fungal acne.
Fungal acne looks like little whitehead clusters on your t-zone and, unlike regular acne, feels itchy. Fungal acne can be brought on by almost any change— in environment, diet, skincare routine, or medication. Yeast usually thrives in warm, wet environments, or with sugars and carbohydrates, so any introduction of these elements may be a factor. (See? No fun.)
The best ways to treat fungal acne are:
Wear breathable fabrics and remove clothes after workouts or sweating.
Try dandruff shampoos to cleanse and antifungal creams (yes like for athlete’s foot) to treat.
Use chemical exfoliants to keep pores clear. Products with salicylic acid, lactic acid or bakuchiol are excellent.
Avoid (most) oils on your face. MCT, Mineral, or Squalane oils are the only safe oils to use.
Try a refrigerated Soon’s Micro-hole Hydrogel Hydrating Face Mask the hyaluronic acid maintains moisture and niacinamide aids compromised skin barrier and overproduction of oil.
